The Department of Noncommunicable Diseases and Mental Health (NMH) is responsible for promoting, coordinating, and implementing technical cooperation activities related to the prevention, control, and surveillance of noncommunicable diseases, all forms of malnutrition, mental health, neurological and substance use disorders, including their risk factors. It also promotes policies and strategies related with disabilities and rehabilitation, road safety, as well as prevention of and response to violence in all its forms.
NMH raises political, public, and professional awareness and helps policymakers, health authorities, practitioners, and communities to understand the burden of the NCDs, all forms of malnutrition, external causes, risk factors, and the impact of the social and commercial determinants of health.
NMH promotes multi-sector and multi-stakeholder strategies that strengthen the capacity of Member States to promote and protect health through public policies, programs, services, and surveillance, to prevent and control risks, improve prevention, diagnosis, treatment, and self-management to reduce the burden of death and disabilities and improve the physical, mental, and social well-being of the population.
NCDs in the Region of the Americas: celebrating PAHO’s 120 years
AREAS OF WORK
CAMPAIGNS
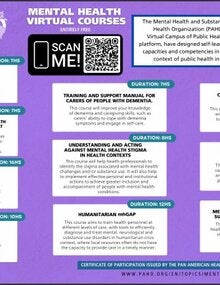
Virtual Courses
Virtual Course on Fundamentals of Palliative Care - 2020
Psychological First Aid (PFA) in disaster management in the Caribbean - 2019
Tobacco and Public Health: From Theory to Practice (2016 Version)
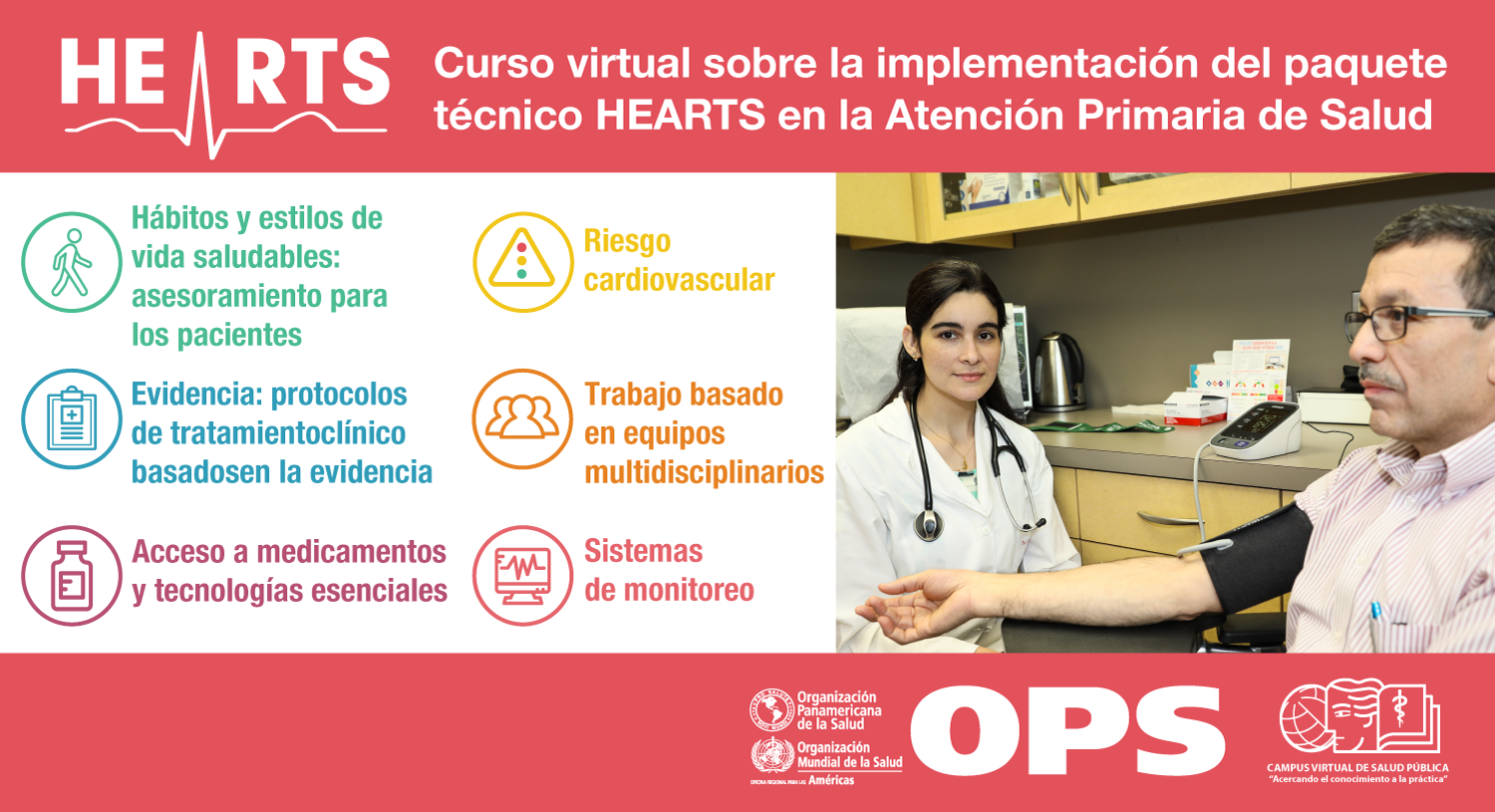
Implementation of the HEARTS Technical Package in Primary Health Care
Preventing Self-harm/suicide: Empowering Primary Health Care providers
Virtual Course on Comprehensive Cervical Cancer Control
Alcohol Use, Women’s Health and Pregnancy: Comprehensive Approaches to Preventing Problems Associated with Prenatal Alcohol Exposure
Newsletter
Subscribe to the PAHO´s email list to receive the Newsletter on noncommunicable diseases and mental health and invitations to webinars and other activities
Latest issue
Special Issue: International Childhood Cancer Day
Past issues
2022
- Special Issue November: International Day for the Elimination of Violence Against Women
- October 2022
- September 2022
- June 2022
- May 2022
- Special Issue May 2022: World No Tobacco Day
- Special Issue May 2022: World Hypertension Day
- April 2022
- March 2022
- February 2022
- Special Issue February 2022: World Cancer Day: Close the care gap
Strategic Partners: PAHO/WHO Collaborating Centres