SUBMENU
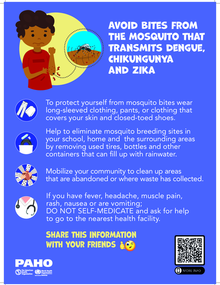
Neglected ('forgotten') diseases and vector-borne diseases are a set of infectious diseases, that primarily affect the most vulnerable populations. These populations include those with the least access to health services, especially impoverished people living in remote rural areas and urban shantytowns, although some of these diseases, such as dengue, zika and chikungunya, also affect large urban areas.
Dealing with these poverty-related diseases requires a more integrated and multi-disease approach that includes multisectoral action, piggy-backed initiatives, and cost-effective interventions to reduce the negative impacts that these diseases have on the health, social, and economic well-being of all people in the Americas.
The Neglected, Tropical and Vector Borne Diseases Unit, part of the Department of Communicable Diseases and Environmental Determinants of Health (AD/CDE), is the group inside PAHO assigned to the area of infectious disease, surveillance, prevention, and control.