In many countries, cancer is the second leading cause of death in children over 1 year of age, exceeded only by accidents. Fortunately, in recent years a great progress has been made in the treatment of childhood cancer. For example, acute leukemia that 30 years ago was considered inevitably fatal, at present, is the most frequent childhood cancer with a five-year survival exceeding 70%. Significantly, most patients can be cured.
Also, similar advances has been made in treatment of solid tumors; since, methods with radioation therapy, surgery and chemotherapy have been used in combination, long-term survival of childhood cancer has significantly increased. Kids are different than adults and it is important, in general, to take action to any different sign or symptoms noted. In summary, while pediatric cancer can not be preventable, the goal of early detection can be achieved by health providers who do a comprehensive medical history, good medical exam, and believe in the parents.
Cancer is a leading cause of death for children and adolescents around the world and approximately 274,000 children aged 0 to 19 years old are diagnosed with cancer each year.
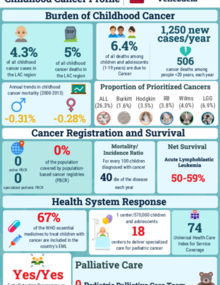
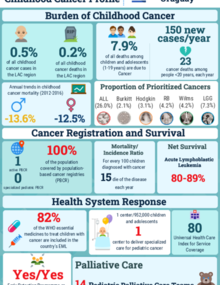
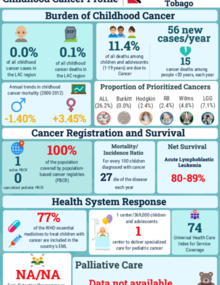
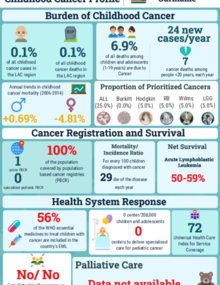
In Latin America and the Caribbean, it is estimated that around 30,000 children and adolescents under 19 years-old will be affected by cancer each year. Of them, almost 10,000 will die due to this disease.
Childhood cancer include a number of different types of tumours that develop in this population group. The most common categories of childhood cancers include leukemias, brain cancers, lymphomas and solid tumours, such as neuroblastoma and Wilms tumour.
In general, in childhood cancer there is no primary prevention or detection through screening.
In high-income countries, more than 80% of children with cancer are cured, but in many low- and middle-income countries the cure rate is only about 20%
Avoidable deaths from childhood cancers in low- and middle-income countries result from lack of diagnosis, misdiagnosis or delayed diagnosis, obstacles to accessing care, abandonment of treatment, death from toxicity, and higher rates of relapse.
The impact of childhood cancer translates into years of life lost, greater inequalities and economic difficulties. This can and should change.
WHO Global initiative for childhood cancer
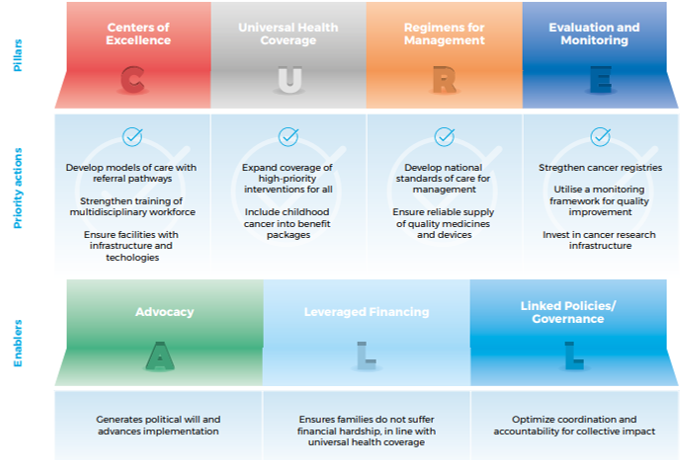
In September 2018 WHO announced a new effort – the WHO Global Initiative for Childhood Cancer – with the aim of reaching at least a 60% survival rate for children with cancer by 2030, thereby saving an additional one million lives. This new target represents a doubling of the global cure rate for children with cancer. The aims of the Initiative are two-fold: to increase prioritization of childhood cancer through awareness raising at global and national levels and to expand the capacity of countries to deliver best practice in childhood cancer care. Concretely, WHO will support governments to assess current capacities in cancer diagnosis and treatment including the availability of medicines and technologies; set and cost priority cancer diagnosis and treatment programmes; and integrate childhood cancer into national strategies, health benefits packages and social insurance schemes (CureAll).
Technical package
Types of cancer prioritized
The WHO Global Initiative on Childhood Cancer focus on six types of cancer:
Acute Lymphoblastic Leukemia
Hodgkin Lymphoma
Retinoblastoma
Wilms Tumor
Burkitt Lymphoma
Low-Grade Glioma
What PAHO does
CureAll Americas represents multi-stakeholder action to improve care and outcomes for all children and adolescents with cancer in Latin America and the Caribbean, within the framework of the WHO Global Initiative against Childhood Cancer.
The CureAll Americas technical package guides countries to implement the Initiative. The results that are expected to be achieved are stronger health systems and better care for children and adolescents suffering from cancer.
The Initiative has multiple stakeholders who have agreed to help governments create strategic plans and priorities. Success will be possible when leading academic centers, professional societies, parent groups, nonprofit foundations, and the private sector come together with a common goal.
In efforts to strengthen the health system response to childhood cancer, the Pan American Health Organization, together with St. Jude Children’s Research Hospital are collaborating with the Ministries of Health, pediatric oncologists, and foundations to develop National Childhood Cancer Plans, in alignment with the Global Initiative for Childhood Cancer (GICC) of the World Health Organization