Public health in the region faces new challenges such as the reemergence of infectious diseases and changes in political, social and economic aspects that determine the health and health equity of the population. These add to persistent challenges related to weaknesses in health systems.
To face these challenges, health authorities, at all institutional levels and together with civil society, are committed to developing a set of capacities to strengthen health systems and guarantee full exercise of the right to health, acting on risk factors and social determinants that have an effect on the health of the population.
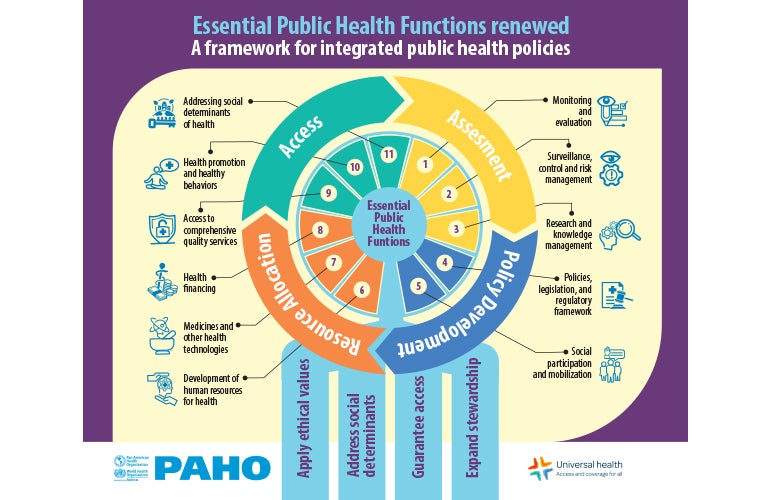
These capacities are framed in different stages of the policy cycle: assessing the health status of the communities and the factors of poor health, developing policies to strengthen health systems and address the determinants, allocating the necessary resources, and guaranteeing access to all public health interventions and services.
- On average, about one-third of people in countries of the Americas (29.3%) reported forgoing needed care due to multiple access barriers.
- Of those who reported forgoing needed care, 17.2% attributed their decision to organizational issues (i.e. long waiting times, inappropriate hours of operation, cumbersome administrative requirements).
- Financial barriers were reported in 15.1% of cases, inadequate availability of resources (i.e. health personnel, medicines, and inputs) was cited in 8.4% of episodes and geographic barriers in 5.4% of cases.
- Importantly, 8.0% attributed their decision to acceptability issues (i.e. language barriers, lack of trust in health personnel, or being mistreated by personnel, preference for traditional and indigenous medicine).
- People in the poorest wealth quintile were more likely to experience barriers related to acceptability issues, financial and geographic access, and availability of resources.
Source: Leveraging household survey data to measure barriers to health services access in the Americas
What are the renewed essential public health functions?
The essential public health functions (EPHF) are the capacities of health authorities, at all institutional levels and together with civil society, to strengthen health systems and guarantee the full exercise of the right to health, acting on the risk factors and social determinants that have an effect on the health of the population. This renewed proposal has an institutional perspective in terms of the capacities of the State and society to perform essential functions to protect the health of the population. Another outstanding feature of the definition is the recognition of the health authorities as the main subject responsible for the exercise of the EPHF at all institutional levels.
This renewed proposal of the EPHF seeks to guide the development of public health policies through intersectoral collaboration during four stages that are part of an integrated policy cycle: evaluation, policy development, resource allocation, and access. It also introduces a new paradigm for public health based on four action-oriented pillars: i) Apply ethical values of public health to address health inequities and their causes. ii) Address the social, economic, cultural, and political conditions that determine the health of populations, iii) Guarantee universal access to comprehensive, integrated, individual, and collective public health services and, iv) Expand the stewardship role of the health authorities to address public health challenges.
PAHO provides technical cooperation on the essential public health functions related to assessment, policy development, resource allocation, and access; to strengthen health systems, particularly to prevent, detect, assess, evaluate, and respond to public health events; and to promote the adoption of integrated, multisectoral approaches to achieve universal health.
It promotes the exchange of knowledge, good practices and cooperation for the strengthening of the essential functions of public health and health systems.