La confiance est le fondement des programmes de vaccination. Lorsque les populations font confiance à leurs prestataires de santé, au système de santé et au ministère de la Santé de leur pays, elles sont plus susceptibles de suivre leurs recommandations en matière de vaccination. Cependant, lorsque cette confiance est érodée ou rompue, l’adoption des vaccins peut faiblir, et exposer ainsi les populations à des maladies évitables par la vaccination.
L’une des mesures les plus importantes que les gouvernements peuvent prendre pour renforcer la confiance dans la vaccination est de suivre les principes de la communication sur les risques et la mobilisation communautaire. En l’absence de communication claire, les rumeurs sur les risques de la vaccination, la méfiance à l’égard des programmes de vaccination, et le refus des vaccins ou la réticence à se faire vacciner peuvent s’intensifier. Le fait de ne pas communiquer efficacement au sujet de la vaccination et de ne pas répondre aux préoccupations de la population peut avoir de graves répercussions sur la réputation des programmes de vaccination et sur le système de santé dans son ensemble, entraîner une chute de l’acceptation et de l’adoption des vaccins et accroître le risque d’éclosions de maladies évitables par la vaccination au sein des groupes de population sous-vaccinés.
Principes de la communication sur les risques et la mobilisation communautaire en faveur de la vaccination
Le respect des principes du Cadre stratégique de communication de l’OMS (en anglais) permet d’améliorer la communication sur les maladies à prévention vaccinale ainsi que sur la vaccination :
Il est essentiel de faire participer les communautés pour comprendre leurs besoins et leurs points de vue concernant la vaccination. De plus, la collaboration avec les communautés permettra aux programmes de vaccination de mettre sur pied des services de vaccination de meilleure qualité et d’améliorer les systèmes et les politiques.
Le document de l’OMS intitulé Programmes de vaccination sur-mesure à l’aide d’un design centré sur l’humain : un guide pratique peut être utilisé pour inciter les communautés à reconnaître les obstacles à la vaccination, à concevoir et mettre en œuvre des interventions pour y remédier, ainsi qu’à les évaluer et les ajuster si nécessaire.
Gestion des fausses informations sur la vaccination
Les fausses informations sur la vaccination ont des répercussions très concrètes sur l’adoption des vaccins. La mésinformation et la désinformation sur les vaccins peuvent ébranler la confiance du public à l’égard des programmes de vaccination systématique et des nouveaux vaccins. Des études ont montré que l’exposition à une mésinformation négative sur les vaccins, même seulement pendant 5 à 10 minutes, augmente la perception des risques vaccinaux et est associée à une probabilité inférieure de se faire vacciner. L’exposition à de fausses informations sur les risques vaccinaux peut amener les gens à percevoir des risques qui n’existent pas (ou qui sont extrêmement faibles).
Le personnel de communication qui soutient les programmes nationaux de vaccination doit investir dans des activités d’écoute sociale sur diverses plateformes afin de comprendre ce que le public pense et dit de la vaccination. Ces informations peuvent ensuite être utilisées pour prendre des mesures visant à corriger les fausses informations par le biais du désamorçage et de la démystification.
Combating false information on vaccines:
|
| The document "Combating False Information on Vaccines: A Guide for Health Workers" is designed to help health workers address vaccine misinformation. It begins by defining misinformation and explaining why it spreads rapidly, often due to its emotional appeal and simplistic explanations. The guide identifies common sources of vaccine misinformation, including influential individuals who profit from spreading false information. The document outlines strategies for combating misinformation, emphasizing the importance of health workers as trusted sources. It provides tips for identifying misinformation online, such as checking URLs, dates, and author credentials, and recognizing tactics like evoking strong emotions or pushing conspiracy theories. Two main approaches to fighting misinformation are discussed: prebunking and debunking. Prebunking involves warning individuals about potential misinformation before they encounter it, while debunking aims to correct false information after it has been consumed. The guide offers practical examples for both methods. Additionally, the document highlights the role of health workers in supporting peers and patients to trust immunization. It suggests being kind, nonjudgmental, and transparent when addressing concerns, and using motivational interviewing techniques to understand and respond to patients' doubts. Overall, the guide emphasizes the critical role of health workers in maintaining trust in vaccines and provides comprehensive strategies to identify, address, and prevent the spread of vaccine misinformation in clinical and community settings. The guide is a valuable resource for health workers to enhance their ability to combat vaccine misinformation, support informed decision-making, and promote trust in vaccines within their communities, and it addresses a pressing issue with practical solutions, supports trusted health workers, and ultimately aims to protect public health by promoting accurate information and trust in vaccines. |
The document "Combating False Information on Vaccines: A Guide for EPI Managers" is designed to help Expanded Program on Immunization (EPI) managers address vaccine misinformation. It begins by defining misinformation and explaining why it spreads rapidly, often due to its emotional appeal and simplistic explanations. The guide identifies common sources of vaccine misinformation, including influential individuals who profit from spreading false information. The document outlines strategies for combating misinformation, emphasizing the importance of EPI managers as trusted sources. It provides tips for identifying misinformation online, such as checking URLs, dates, and author credentials, and recognizing tactics like evoking strong emotions or pushing conspiracy theories. Two main approaches to fighting misinformation are discussed: prebunking and debunking. Prebunking involves warning individuals about potential misinformation before they encounter it, while debunking aims to correct false information after it has been consumed. The guide offers practical examples for both methods. Additionally, the document highlights the role of EPI managers in supporting health workers to trust immunization. It suggests being kind, nonjudgmental, and transparent when addressing concerns, and using motivational interviewing techniques to understand and respond to health workers' doubts. The guide also emphasizes the importance of creating a supportive environment for health workers, promoting pro-vaccine norms, and providing continuing education on vaccines. Overall, the guide aims to help EPI managers maintain trust in vaccines and provides comprehensive strategies to identify, address, and prevent the spread of vaccine misinformation in clinical and community settings. This document is necessary to equip EPI managers with the knowledge and tools to combat vaccine misinformation, support their teams, and promote trust in vaccines, ultimately protecting public health. |
| False information about vaccines and vaccination – whether it is spread intentionally (known as disinformation) or not (known as misinformation) – poses a serious threat to public health in the Americas. Multiple studies have shown that exposure to vaccine-related misinformation can shake population trust in the Expanded Program on Immunization (EPI) and negatively impact individuals’ attitudes and intentions toward vaccination, even among individuals who have previously been vaccinated. Unsurprisingly, misinformation that implies vaccination causes harm and that sounds scientifically credible has shown to be more likely to deter individuals from intending to get vaccinated. Fighting back against science deniers and their misinformation is a critical part of maintaining trust in immunization and protecting populations from a variety of vaccine-preventable diseases (VPDs). Critical in this fight are understanding how and why misinformation spreads; which approaches can be employed to combat it, both before and after people have been exposed; and rebuilding trust in immunization after it has been shaken. Ministry of Health risk communication and community engagement (RCCE) teams face a daunting task in staying abreast of misinformation, so they are able to monitor it and take decisive action to combat it when needed. By collaborating at the national, district, and local levels with a variety of partners – including health workers (HW), who have been repeatedly shown to be the most trusted source of information on vaccines and vaccination – RCCE teams can use several different approaches to equip their audiences with the tools and knowledge to resist misinformation. |
The document "Combating False Information on Vaccines: A Guide for Educators" aims to help educators address vaccine misinformation. It begins by defining misinformation and explaining why it spreads rapidly, often due to its emotional appeal and simplistic explanations. The guide identifies common sources of vaccine misinformation, including influential individuals who profit from spreading false information. The document outlines strategies for combating misinformation, emphasizing the importance of educators as trusted sources. It provides tips for identifying misinformation online, such as checking URLs, dates, and author credentials, and recognizing tactics like evoking strong emotions or pushing conspiracy theories. Two main approaches to fighting misinformation are discussed: prebunking and debunking. Prebunking involves warning individuals about potential misinformation before they encounter it, while debunking aims to correct false information after it has been consumed. The guide offers practical examples for both methods. Additionally, the document highlights the role of educators in supporting students and their families to trust immunization. It suggests being kind, nonjudgmental, and transparent when addressing concerns, and using motivational interviewing techniques to understand and respond to students' doubts. The guide also includes lesson plan ideas and video discussion questions to help educators integrate these strategies into their classrooms. Overall, the guide emphasizes the critical role of educators in maintaining trust in vaccines and provides comprehensive strategies to identify, address, and prevent the spread of vaccine misinformation in educational settings. It provides educators with the knowledge and tools to identify and combat vaccine misinformation effectively. This is crucial as educators are trusted sources of information and can influence students and their families positively. |
| Journalists play a critical role in keeping the public up to date on information they need to be healthy, including staying current on their vaccines. Along with health workers, the media is one of the most trusted sources the public have for scientific information; journalists help shape perceptions, attitudes, and even behaviors. This document aims to support journalists, regardless of their medium, to accurately cover stories related to vaccines and vaccination. Journalists play a critical role in keeping the public up to date on information they need to be healthy, including staying current on their vaccines. Along with health workers, the media is one of the most trusted sources the public have for scientific information; journalists help shape perceptions, attitudes, and even behaviors. While misinformation about vaccination is as old as vaccines themselves, its more recent explosion, especially on social media, has caused concern for health professionals and scientists. Studies have demonstrated that even brief exposure to vaccine misinformation can negatively impact individuals’ attitudes and intentions toward vaccination, even among people who have previously been vaccinated. As vaccination coverage rates fall, populations are left exposed to deadly vaccine-preventable diseases (VPDs) like measles, pertussis (whooping cough), polio, tetanus, and others. Keeping people healthy and protected from VPDs requires collaboration across sectors, especially in the face of vaccine misinformation. For this reason, PAHO has created this document for media professionals covering vaccination, which covers bias and balance, norms and perceptions, and tips on other related topics, as well as additional resources for further information. |
| Have you seen or heard something about vaccines online that has made you do a double take? There is no shortage of vaccine misinformation out there, from wild conspiracy theories to small pieces of the truth that have been distorted or blown out of proportion. What is true though, is that the overwhelming majority of scientists and medical experts agree that vaccines are safe and effective, and that not being vaccinated puts you and your loved ones at risk of deadly diseases that could start to make an appearance again if not enough people are vaccinated. Because even a brief exposure to misinformation about vaccines can impact a person’s decision to get vaccinated, it is important that we all do our part to stop its spread. As a content creator on social media, you can learn tips and tricks on how to spot misinformation and share them with your followers. By doing so, you will be making the world a healthier and safer place – and who does not want that? |
Désamorçage
Démystification
Avec le désamorçage comme avec la démystification, l’écoute sociale est essentielle pour comprendre ce que le public dit de la vaccination et les rumeurs qui circulent et pourraient avoir des répercussions sur l’adoption des vaccins.
Pour en savoir plus sur la gestion des fausses informations liées à la vaccination, consulter la publication de l’OPS intitulée Communication sur les risques liés à la vaccination. Elle propose des exemples pratiques et concrets de ce qu’il faut faire ou ne pas faire relativement aux processus et aux principes de communication sur les risques et de mobilisation communautaire, aux messages, à la perception des risques, à la gestion des fausses informations, à la collaboration avec les partenaires et à la pharmacovigilance.
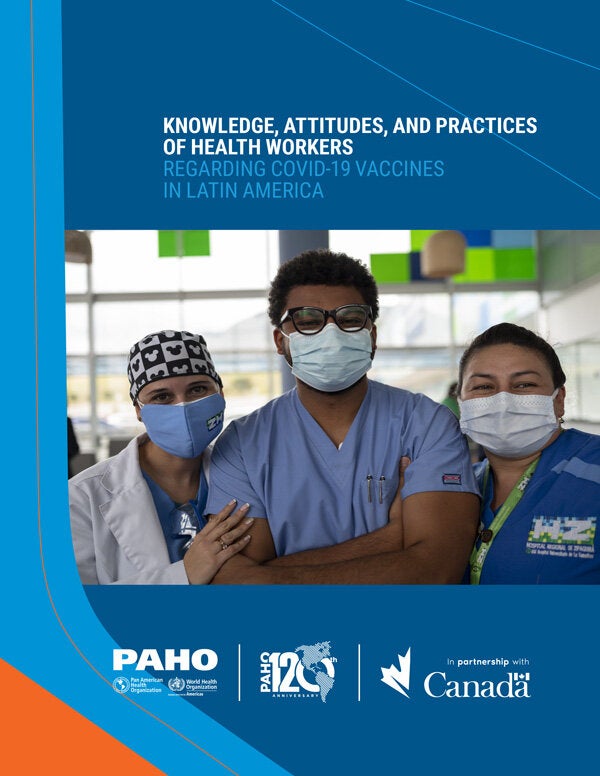
Personnel de santé et vaccination
Les agents de santé sont toujours considérés comme les sources d’information les plus fiables sur la vaccination. Les recommandations des agents de santé en faveur de la vaccination peuvent avoir des retombées considérables sur l’adoption des vaccins. Cependant, pour que ces recommandations aient un effet optimal, ils doivent les présenter avec empathie, en délivrant des informations factuelles et en gardant à l’esprit une perspective culturelle et les obstacles potentiels liés à la culture. Pour cette raison, l’OPS encourage fortement les programmes nationaux de vaccination à investir dans leurs agents de santé en les formant à la communication interpersonnelle sur la vaccination. Outre les formations, les programmes nationaux de vaccination devraient élaborer des outils et des aides visuelles pour s’assurer que les agents de santé disposent des connaissances scientifiques nécessaires pour répondre à des demandes de conseils sur la vaccination de la part des clients et des membres de la communauté.
De même, le personnel de communication sur la santé devrait envisager d’élaborer des campagnes, des stratégies et des interventions particulières, ou au moins des messages ciblés ayant fait l’objet de tests auprès du public, à l’attention des agents de santé, afin d’insister sur les points clés qu’ils doivent garder à l’esprit lorsqu’ils doivent communiquer avec les clients et le grand public sur des questions liées à la vaccination.