About Us
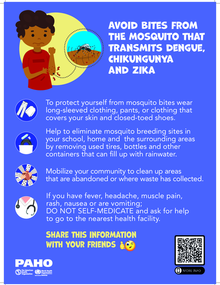
Communicable Disease Prevention, Control, and Elimination promotes, coordinates, and implements technical cooperation activities directed toward the surveillance, prevention, control, elimination and/or reduction of communicable diseases, zoonoses that are technically sound and appropriate for the political and sociocultural context in which they are implemented. It strives to achieve a sustainable impact on health by providing normative guidance, furthering the implementation of evidence based interventions, fostering alliances that strengthen country capacity, improving the effectiveness of inter-country collaboration, and facilitating policy and decision-making processes.
Strategic Partners: PAHO/WHO Collaborating Centres