In an effort to re-visit and revitalize PAHO's vision and approach to community health, an Expert's meeting was held in June in Washington, DC, gathering participants working within the field of community health in 14 different countries in the Americas, as well as personnel representing a variety of departments within PAHO. The results of the meeting included a set of inputs and recommendations that will hopefully help PAHO propel forward in its pursuit of a community health strategy that is adapted to meet the Region's health needs in the 21st century.
Washington D.C., June 14-16 2017
Executive summary
In an effort to re-visit and revitalize PAHO's vision and approach to community health, an Expert's meeting (agenda) was held in June in Washington, DC, gathering participants working within the field of community health in 14 different countries in the Americas, as well as personnel representing a variety of departments within PAHO. The results of the meeting included a set of inputs and recommendations that will hopefully help PAHO propel forward in its pursuit of a community health strategy that is adapted to meet the Region's health needs in the 21st century.
Background
Over the past two decades, countries in the Latin America and the Caribbean (LAC) Region have experienced significant demographic and epidemiological changes. Under-five and maternal mortality has fallen though inequities remain. Fertility is lower while life expectancy has increased, yet overall quality of life has not necessarily improved. Countries have seen rapid shifts in population settings from rural to urban cities giving rise to new health challenges across the life course. Chronic diseases and mental health issues are on the rise, while infectious diseases persist. At the same time, technological innovations are creating new opportunities for approaching population and individual health. Recognizing that bio-medical interventions are not sufficient to address these health challenges, this meeting explored the changing dynamics of communities and discussed how community health approaches could be applied to meet the Region's health needs in the 21st century.
Objectives
- To review the evolution of communities and community health
- To better understand how community health practices can be used to better respond to the specific health challenges facing communities today
Day 1, June 14
Dr. Carissa F. Etienne, Director of PAHO, opened the meeting with a history of community health from the Declaration of Alma Ata in 1978 through the unfinished agenda of the Millennium Development Goals and the need for people- and community-centered health systems to meet the targets of the Sustainable Development Goals (SDGs) and Universal Health Coverage. Dr. Etienne began the meeting with the following 6 questions:
1. How can we as an organization meaningfully take action in this era to implement the concept of people and communities at the center of health systems strengthening?
2. How can we make the system work for the various communities that it must serve?
3. How do we ensure social mobilization and community empowerment for health?
4. How do we amplify prevention and promotion programs within communities? How can we ensure their place at the table? What are tools and approaches for doing that?
5. How can we help communities to be proponents and actors of their own health and not just passive recipients?
6. How do we define within PAHO, programs that work with national and local governments to truly empower communities?
"Our member states wanted us to look at the public health aspect of care and the communities as proponents of their own health. This is an opportunity for us to do that. How to link public health and how to link community health with health systems strengthening based on primary health care, SDGs, Leave No One Behind- it is important for us to do this."
-Dr. Carissa Etienne, Director of PAHO
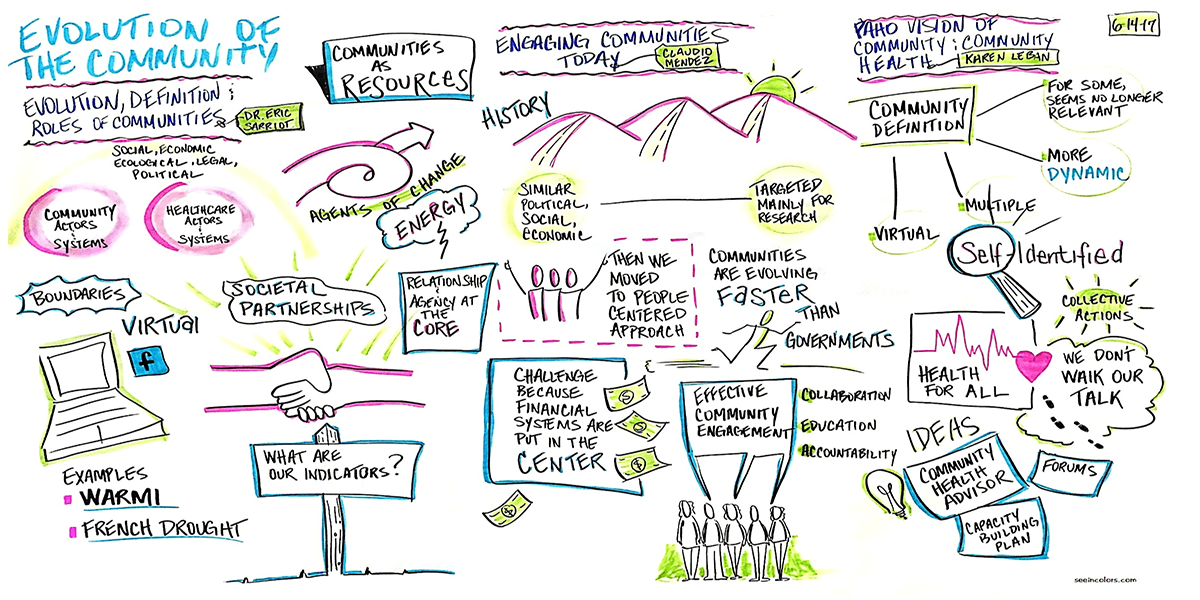
Dr. Eric Sarriot, Sr. Health Systems Strengthening Advisor, Save the Children, presented "The Evolution, Definition, and Role of Communities." He proposed four possible lenses through which to view a community's role: as a beneficiary, a resource, an agent of change, or a political power center. Each lens affects the community health strategy.
Dr. Claudio Méndez, Associate Professor of Health Policy, Universidad Austral de Chile, stressed the importance of community engagement during his presentation. Communities are seeking solutions beyond health systems and the health sector is no longer the main entry point for community health and wellbeing. Furthermore, communities are evolving faster than governments and their social policies, which is why it is crucial to engage communities in the political process.
Ms. Karen LeBan, International Consultant, presented PAHO'S Current Vision of Community and Community Health based on interviews with 25 personnel working at PAHO. Personnel agreed that a community reflects the places where people live, work, play, pray, study, or share common beliefs or needs; and that a community health approach should address geographical and virtual spaces. A community health approach is concerned with health of all the people across the life course; and needs to reflect the diversity of the Region's peoples. They also agreed that this was an opportune time to strengthen Community Health within PAHO to achieve organizational goals.
Dr. Hector Carrasco, D.Ph. Candidate at Harvard T.H Chan School of Public Health, presented "What do we mean by community health in the 21st century?," stressing the shift from 'down-stream solutions' to 'up-stream solutions' focused on interdependence, advocacy and activism, and professional community health workers. Community health should have four pillars: innovative financing mechanisms, intersectoral collaboration, transformative bio-social and advocacy training, and professional change agents with clear career pathways.
Dr. Tom Prohaska, CHHS Dean's Office, George Mason University, presented "Using health data and tools to support community actions," calling for the reintegration of medicine, social work, and public health, and reflecting on the importance of healthy ageing and its inclusion of physical environments, communities, and behaviors. All sociodemographic, behavioral and psychosocial risk factors for poor health should be considered in the environments in which they occur. Several major factors should be considered in building healthy communities: direct and indirect impact of policy on health; emerging role of technology; and the growing role of genetics in long-term health outcomes.
Dr. Sheoran Bhupendra, Executive Director, YTH, presented "New approaches in community health for the next decade-Community Health in the Digital Era" reflecting on the new normal: an abundance of content is now being produced and shared at all times online. Youth and young adults in LAC are the most active users of digital media in the world and mobility is key. The challenge for us now is figuring out the best way to use these new technologies in ways that promote community health and community engagement. Communities (both physical and virtual) deserve real information, when they need it, and how they need it.
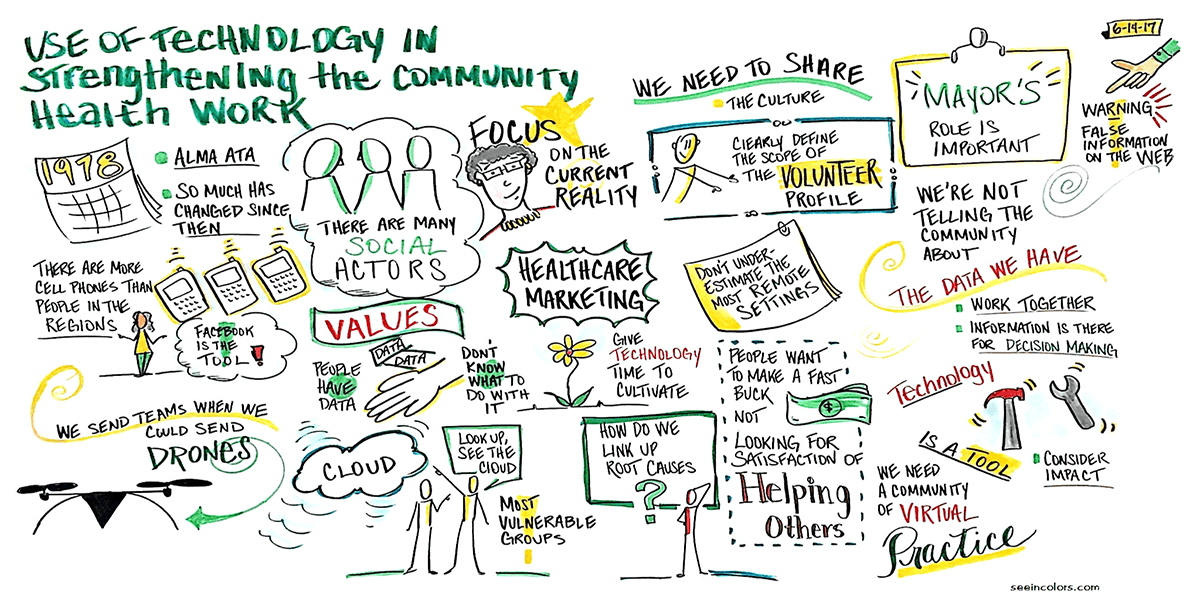
The discussion held during the afternoon concerned the 'use of technology in strengthening community health work.' Together, participants discussed how technology has undergone the biggest transformation in the Region since Alma-Ata, and that we need a leap in order to harness its strengths. On average, over 50% of individuals are connected to the internet in the Americas, and there are currently 108 mobile lines for every 100 people, yet 78% of National Health Authorities lack skilled personnel and have inadequate infrastructure. We need to generate information that is rational, validated, useful, and cost-effective.
Day 2, June 15
Dr. Gina Watson, PAHO Representative in Colombia, led the plenary discussion "Role of Community Health in Post-Conflict Colombia." Community participation has been critical to the peace process. The level of violence against civilians is a priority and working with communities is vital for the victims and their developmental recovery. Strategic alliances with the education sector, local government, mayors, and other social actors, along with an intercultural health approach is helping to rebuild trust, retain health staff, and socialize community leaders and local organizations. Weapons are being collected, and violence against medical staff is decreasing, enabling doctors to return to the area. Panelists of Colombia Representatives presented some experiences of community health work using an integrated and sustainable development approach to strengthen grassroots organizations, which resulted in a decrease in maternal mortality and deaths due to violence in the past year. It was described how the efforts were concentrated on eradicating extreme poverty, strengthening families and empowering communities.
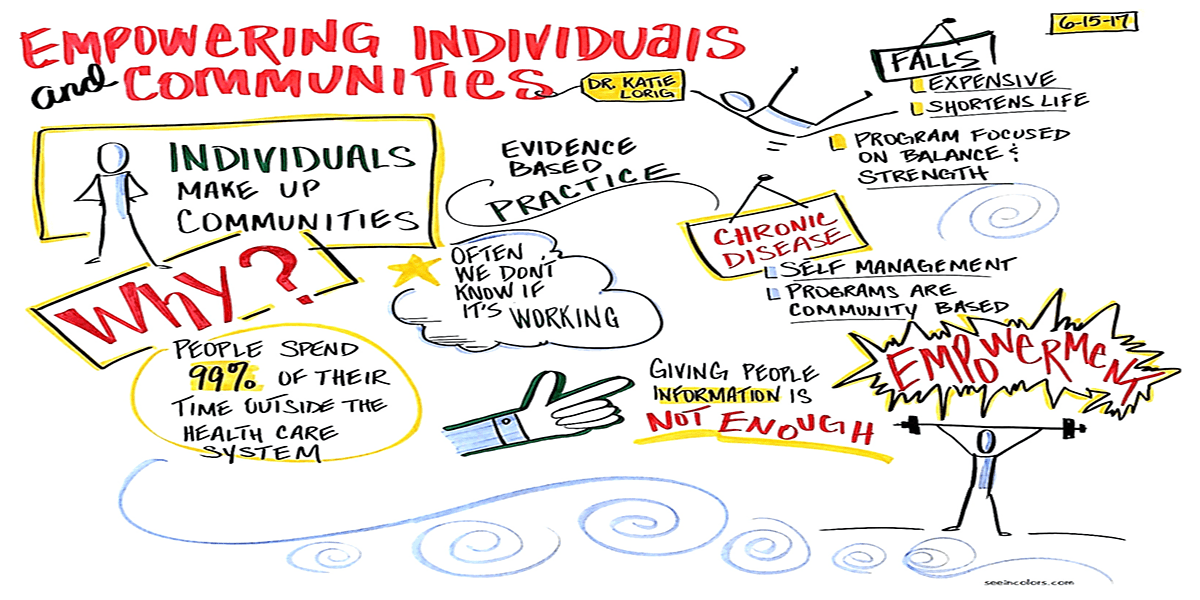
Katie Lorig, Director, Patient Education Research Center at Stanford School of Medicine, presented on "Communities as Part of the Delivery System." People spend 99% of their time outside the health system; what they do during that time determines their health and quality of life. There are many examples of non-traditional community health programs. We should focus on those that are evidence-based, cost-effective, cover the lifespan, and ensure they are adequately funded and supported.
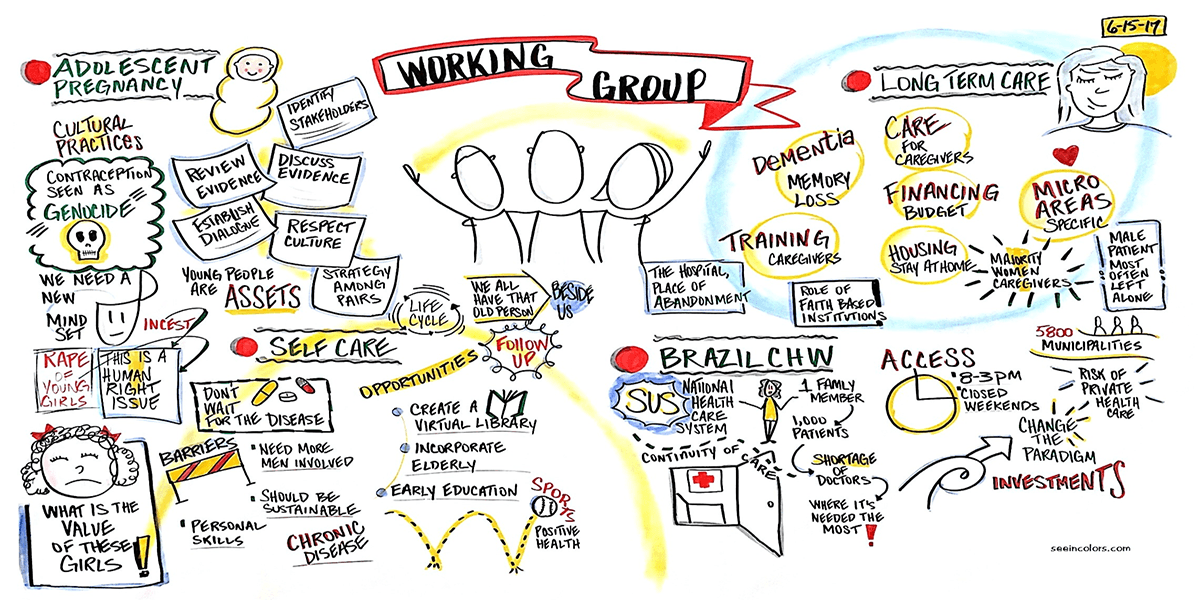
During mid-morning, experts were divided into 4 groups to review 1 Case Study each. The Case studies included: "Leaving No One Behind- Adolescent Pregnancy in Minority Groups," "Self-Care: Chronic Disease Management," "Long-Term Care and Dementia," and "The Human factor in Moving Forward Community Health Work in Brazil."
- Produce intervention strategies incorporating adolescent minorities as agents of change
- Incorporate elderly community into the health system and policies using a human rights approach
- Create inter-disciplinary teams that attend to people at home for long term care reducing institutionalization of service
- Brazil's strategy of family health teams with paid CHWs has made a positive impact on health, but requires political will and continued investment in CHWs and a more concrete career pathway
Day 3, June 16
Dr. Mario Reali, Specialist in Neurology and Psychiatry, started the morning with a presentation on the "Next Steps in Community Health." Dr. Reali spoke about his work in Trieste District, Italy, to establish a community health system structured in a life course manner with local control of the health budget. He explained the organizational structure of the District and how some of the main interventions and functions are integrated with other programs and departments.
Martha Pelaez, International Consultant and Advisor on Aging, presented "Improving Community Health Work in the Next Decade." Improving community health requires large-scale social change, which in turn requires broad cross-sector coordination. This poses a challenge since the health/social sector often remains focused on isolated interventions. To have collective impact in community health, we must have continuous communication, a common agenda, a common vocabulary, mutually reinforcing activities, a shared measurement system, and a funded backbone and support organization (which can be played by PAHO). Results should be based on accountability: How much did we do? (quantity); How well did we do it? (quality); Is anyone better off? (impact)
Dr. Yves Bergevin, Director of Global Health Program, Department of Family Medicine, McGill University, presented on "Community health workforce within health systems." Four complementary strategies are needed for health impact: 1) empowered individuals and families, 2) quality primary care, 3) strong public health, and 4) whole-of-government intersectoral action to address the social determinants of health. All strategies require motivated and competent staff with the appropriate level of skills for the job. A workforce should be skilled, salaried, supervised, supplied, and scaled-up. There is a need to shift from hospital-centric episodic care towards evidence-informed population-based primary and community care with modern family health teams.
Towards Reaching Consensus:
Communities in the Americas today:
- Are no longer defined by their geographical or physical locations
- Spend 99% of their time generating health outside the health system
- Are more connected to the internet
- Provide different solutions to those raised by the health system
- Can evolve faster than governments and their social policies
- Occupy roles as agents of change and political power centers
- Hold the knowledge about local needs and solutions
- For the first time in history, five generations are alive at the same time
- Are experiencing rapid social and demographic transitions
Community health approaches today should:
- Go beyond addressing traditional spaces (e.g. geographical or physical spaces)
- Shift from episodic care towards population based and community care with modern family health teams
- Promote active participation and empowerment of the community in health
- Consider the sociodemographic, behavioral and psychosocial risk factors for poor health in the environments in which they occur
- Take into account the emerging role of technology
- Promote inter-sectoral action and dialogue between local government, health and other professionals, and community representatives
- Function to empower individuals and families
- Cover the lifespan
- Be based on mechanisms for accountability: How much did we do? (quantity); How well did we do it? (quality); Is anyone better off? (impact)
"We must be the catalyst for that change that needs to occur at a global level. I see it as our responsibility to ensure that this can happen."
-Dr. Carissa Etienne, Director of PAHO