Provision of interoperable and secure software for the comprehensive delivery of telehealth services, in accordance with the feasibility analysis conducted by the country or institution.
Collaboration for the implementation and adaptation of the software to existing systems.
Support in identifying institutions with the necessary maturity level to implement telehealth services within the defined period.
Support for implementing telehealth services focused on NCDs as a starting point to progressively expand other remote care services.
Development of strategies to establish asynchronous telehealth services between health teams, based on integrated health service networks.
Support in change management and knowledge transfer through training strategies and educational resources for health teams and patients.
Features
- Asynchronous model: this is the model in which the person who consults and the person who answers are not online. It is generally implemented using structured forms where the request/clinical case is uploaded and answered in a scheduled time in an asynchronous manner. Sometimes files or images can be attache.
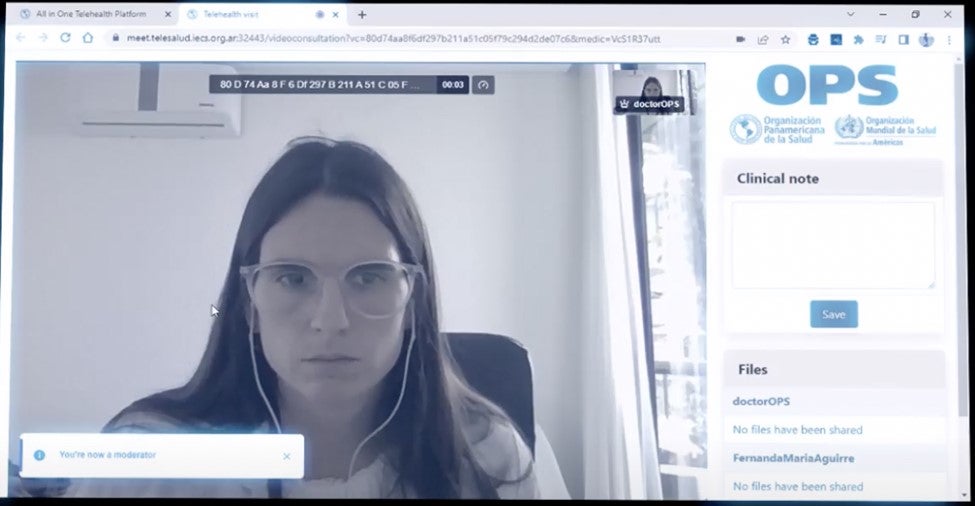
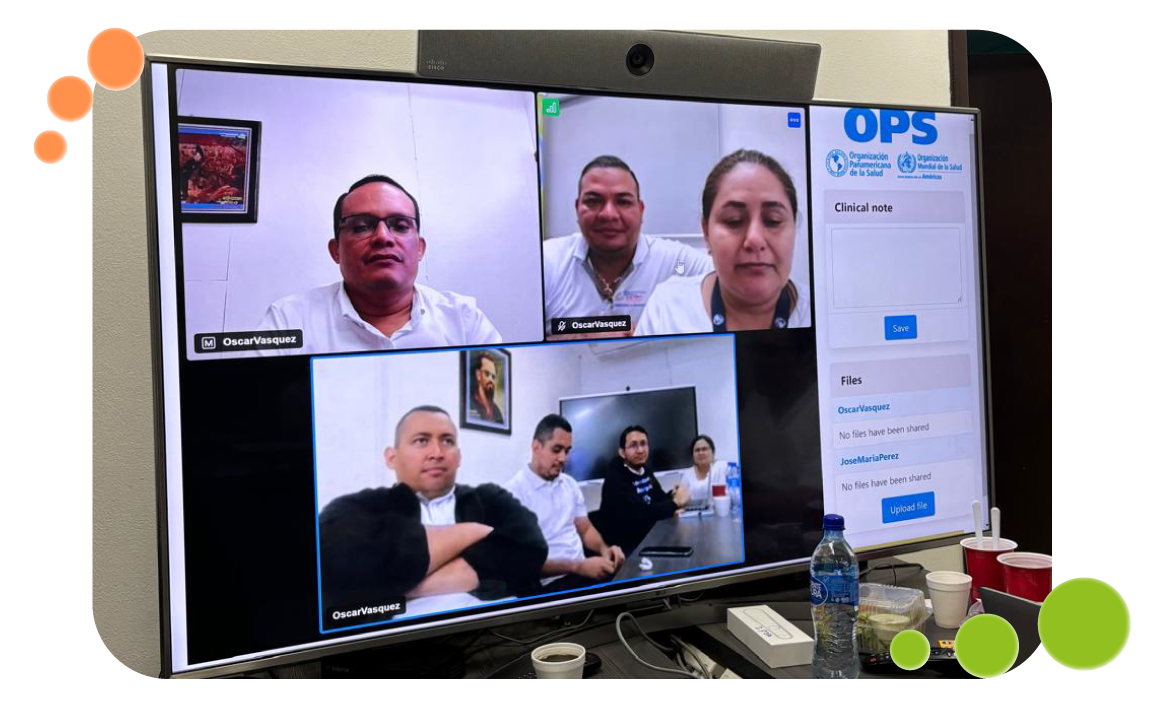
- Synchronous model: the consultation occurs online, with people communicating live. It is generally implemented by teleconference service where audio and video are transmitted. Sometimes files or images can be attached.
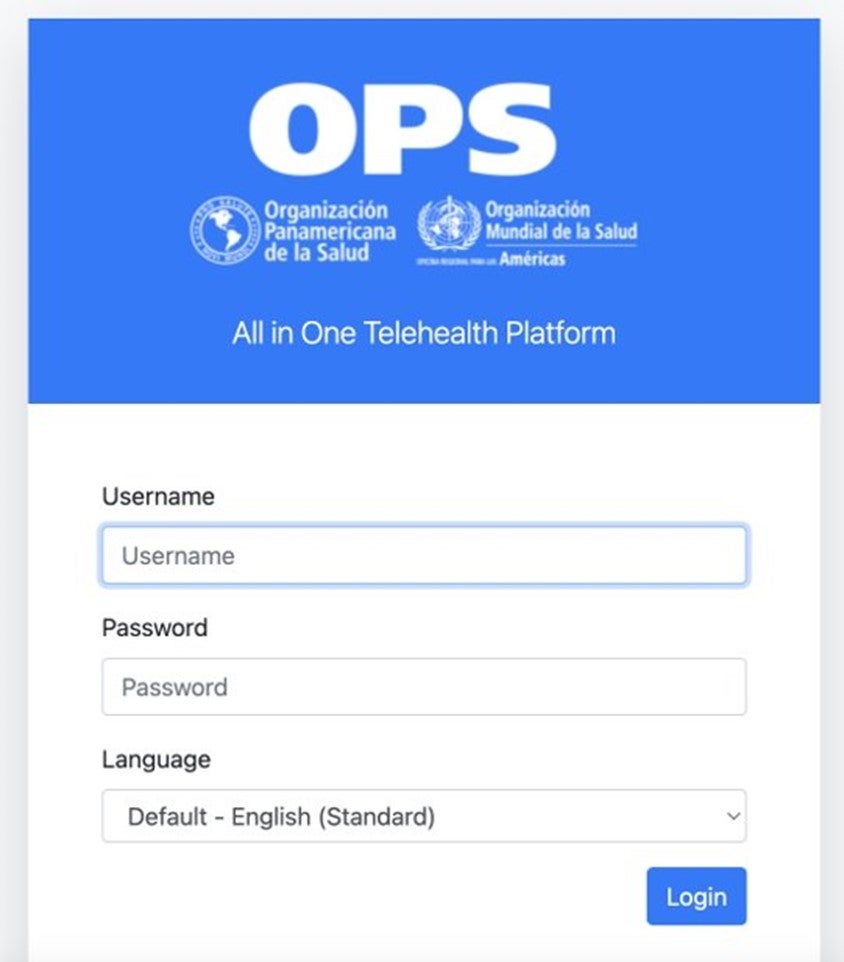
Login to the platform and clinical notes
Type of Services
Patient / health team:
This model of care occurs between a patient or group of patients, or a patient and their family member/caregiver, and a member of the health team. The primary interaction takes place between the patient and the health team.
Professional / professional | second opinion:
This is what we commonly refer to as a second opinion. It occurs between professional teams, generally regarding a specific case, with or without the patient’s presence. The primary interaction is between health teams.
Telemonitoring:
This is a specific use case that can occur online or asynchronously, where a patient typically reports defined variables, such as a vital sign or the progression of a clinical condition. More advanced telemonitoring models can integrate devices so the patient does not need to manually transcribe the data. On the other end, a health team analyzes this information.