Leishmaniasis continues to be a major health problem in four eco-epidemiological regions of the world: the Americas, East Africa, North Africa, and Western and Southeast Asia.
In the Americas, leishmaniasis is a zoonotic vector-borne disease, with a complex transmission cycle involving a wide variety of parasite species, reservoirs, and vectors. It is caused by various species of protozoa of the genus Leishmania and is transmitted to animals and humans through the bite of insects of the Psychodidae family. Its presence is directly linked to poverty, though other social factors, in addition to environmental and climatic factors, directly influence its epidemiology.
In the Region, 15 of the 22 species of Leishmania pathogenic to humans have been identified, and nearly 54 different species of vectors are potentially involved in transmission. The parasite is transmitted through the bite of female sandflies of the subfamily Phlebotominae, popularly known by names such as "chiclera, asa branca, palomilla, mosquito palha, and torito". This insect is active at night, when the parasite is transferred to humans and animals through its bite.
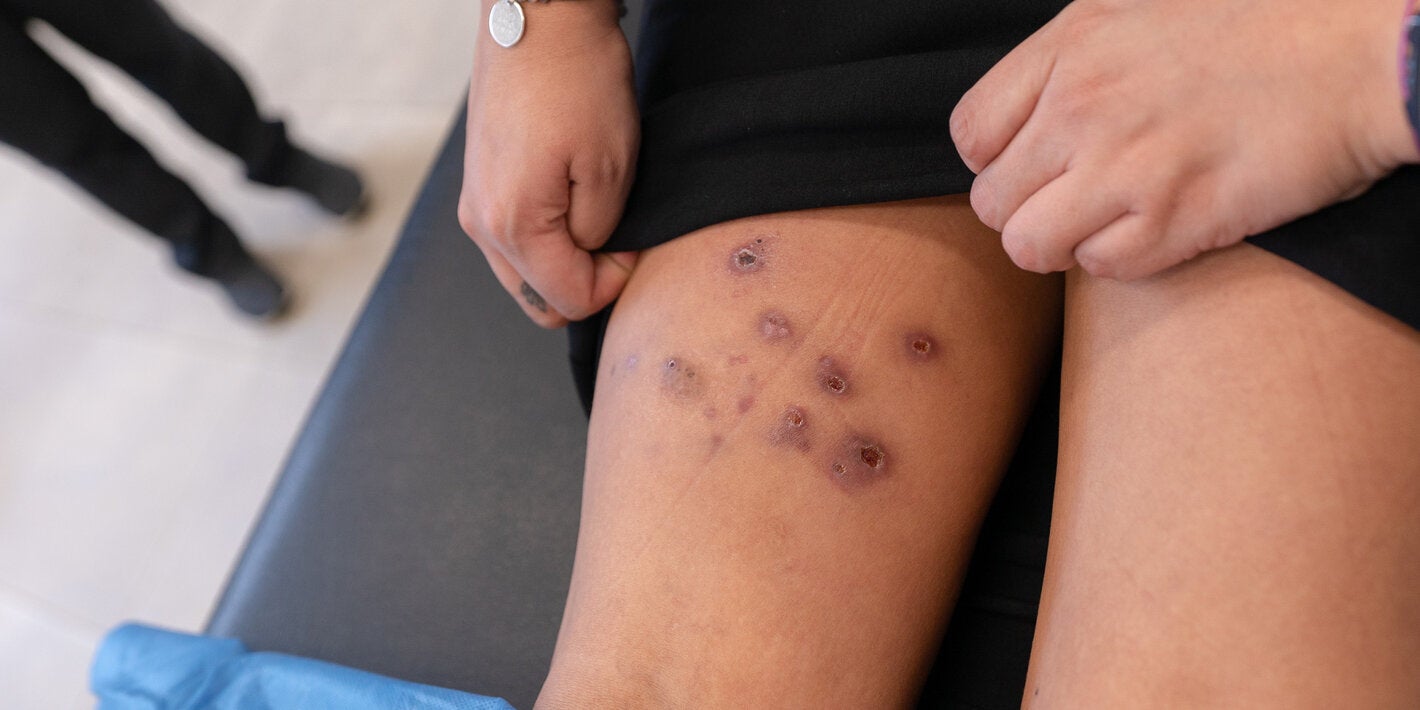
The disease has various clinical manifestations, classified into three forms: cutaneous, mucosal/mucocutaneous, and visceral. Visceral leishmaniasis is characterized by irregular episodes of fever, weight loss, hepatosplenomegaly, and anemia and, if left untreated, causes death in more than 90% of cases. Mucosal/mucocutaneous leishmaniasis, if left untreated, can lead to partial or complete destruction of the mucous membranes of the nose and mouth, which can cause severe disability. Cutaneous leishmaniasis, the most common form of this infection, produces mostly ulcerative lesions that leave lifelong scarring.
Know more about:
- Globally, leishmaniasis is among the top 10 neglected tropical diseases, with more than 12 million people infected.
- Leishmaniasis is endemic in 99 countries, CL in 90 countries, and VL in 80 countries, while in 71 countries the two clinical forms, CL and VL, are endemic.
- Of the 11 countries reporting 90% of CL cases, three are in the Americas: Brazil, Colombia, and Peru.
- Worldwide, four countries account for 60% of cases of visceral leishmaniasis: Brazil, Ethiopia, Kenya and Sudan.
- More than 42 countries report Leishmania-HIV co-infection, intensifying the burden of leishmaniasis, due to the increased difficulty this poses for clinical management and treatment.
- In the Region of the Americas, cases of cutaneous leishmaniasis have been reported from the southern United States to northern Argentina, except for the Caribbean islands, Chile and Uruguay.
- Cutaneous and visceral leishmaniasis are present in 22 countries, and CL is endemic in 19 countries, while VL is endemic in 13 countries.
- In 2001–2023, a total of 1 178 436 cases of cutaneous leishmaniasis (CL) and mucosal leishmaniasis (ML) were reported to PAHO, with an average of 51 236 reported cases per year. In the same period, 73 092 new cases of visceral leishmaniasis (VL) were recorded, with an annual average of 3178 cases and a case fatality rate of nearly 8%, considered the highest rate compared to other continents.
- The available tools for prevention and control are limited, so exposed individuals should take steps to reduce contact with the vector. In addition, health authorities should implement surveillance efforts and, when necessary, carry out public health interventions, taking into account standardized risk stratification for both CL and VL. Early diagnosis and proper treatment are essential to avoid complications caused by the cutaneous and mucosal form, and to reduce the lethality of VL.
- Diagnosis of the disease is essential in order to establish a specific treatment, and to limit the progression of the disease, relieve signs and symptoms, and improve the quality of life of patients. If left untreated, diffuse mucosal and cutaneous forms of the disease can lead to deformity and disfigurement, while the visceral form results in death in more than 90% of untreated cases.
- PAHO/WHO provides technical cooperation to national health authorities, which includes training in disease surveillance, prevention, diagnosis, treatment, and control at the clinical, epidemiological, entomological, and laboratory levels. It also assists in the development of guidelines for the clinical management of patients, epidemiological surveillance, and dissemination of knowledge. In countries where the disease is endemic, PAHO/WHO collaborates in the purchase of medicines, through the Strategic Fund, and also in securing other inputs necessary for the development of disease prevention and control efforts.
- PAHO/WHO is implementing the Plan of Action on Leishmaniasis in the Americas 2023-2030, which seeks to consolidate efforts to achieve the goals of PAHO's Communicable Diseases Elimination Initiative, as well as the WHO Road Map for Neglected Tropical Diseases.