Brazil has received certification from the World Health Organization (WHO) for the elimination of mother-to-child transmission of HIV, becoming the country with the largest population to achieve this certification.
The country demonstrates that elimination at scale is possible when people-centered care guide public health action.
PAHO Celebrates Brazil’s Historic Achievement: Elimination of Mother-to-Child Transmission of HIV
Washington, DC, 19 December 2025 – The Pan American Health Organization (PAHO) congratulates Brazil on achieving the elimination of mother-to-child transmission (EMTCT) of HIV—a landmark accomplishment for public health in the Americas. As the largest country in the world to reach EMTCT, Brazil reaffirms its leadership in universal health coverage through its Unified Health System (SUS).
Recent history of mother-to-child transmission of HIV in Brazil
Over the past two decades, Brazil has made consistent progress toward eliminating mother-to-child transmission of HIV by combining strong public policies, universal access to health services, and sustained investments in prevention and treatment. Despite its large population and regional diversity, the country expanded routine HIV testing during prenatal care and ensured timely access to antiretroviral therapy for pregnant women through its Unified Health System (SUS).
Strengthening Primary Health Care (PHC) as the operational pillar of EMTCT enabled early identification of pregnancy, routine testing, rapid linkage to treatment, and continuous follow-up of pregnant women and HIV-exposed children. Community health workers, home visits, and active case-finding played a key role in reaching populations in situations of greater vulnerability, including those in remote and hard-to-reach areas.
The path toward elimination
Brazil adopted a progressive subnational certification strategy, recognizing states and municipalities that achieved elimination targets using PAHO/WHO tools adapted to the national context. This approach strengthened local organization, promoted greater uniformity in protocol implementation, and ensured national coherence, while allowing flexibility to respond to local realities.
Strategic planning, the strengthening of PHC, and coordination across different levels of government enabled the country to meet all elimination criteria, including a vertical transmission rate below 2% and coverage above 95% for prenatal care, routine HIV testing, and timely treatment of pregnant women and newborns.
The evaluation included data analysis and technical visits to health facilities in different regions of the country and was conducted by an independent global expert committee, with support from the Pan American Health Organization (PAHO).
More Stories
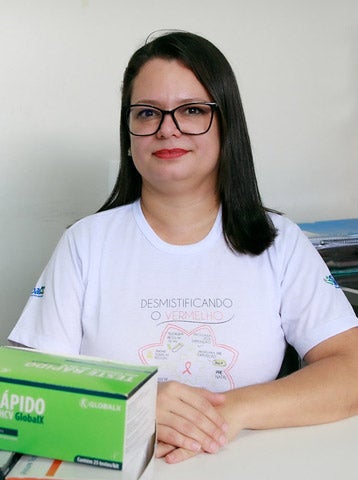
Maria Priscila – Primary Health Care Nurse (Cacoal, Rodônia)
Maria Priscila has worked for more than a decade in prenatal care at the Basic Health Unit (UBS) in Cacoal, where she performs hundreds of rapid tests for HIV, syphilis, and hepatitis every day. She is often the first person to identify a risk—and the first to extend a hand of support. Over the years, she has seen fear turn into reassurance and early diagnoses change the future of many families.
“Rapid testing changes patients’ lives. In 20 minutes, we can provide guidance, make referrals, and lift a huge burden of fear. When women understand that they can have a healthy baby, everything changes.”
Dr. Camila Lira Borges – Infectious Disease Specialist (Salvador, Bahia)
Dr. Camila follows pregnant women living with HIV from their first referral from primary health care services. For her, the moment of diagnosis is decisive—every minute matters to reduce risks and ensure a smooth continuum of care. She highlights the essential role of early testing and the strong coordination between Primary Health Care (PHC) and the Specialized Care Service (SAE).
“Primary health care is fundamental. When we can test and diagnose early, we can start treatment immediately. That is what protects the baby.”
Dr. Alex Acioly – Physician (Cacoal, Rodônia)
At the Specialized Care Service (SAE) in Cacoal, Dr. Alex accompanies pregnant women living with HIV from their first consultation through delivery. His work involves frequent medical visits, health education, and close coordination with obstetricians, psychologists, and nursing staff. He recalls cases of women who arrived overwhelmed and fearful and left reassured once they understood that having a healthy baby was possible.
“It is essential to show that, with proper treatment, a woman living with HIV can have a healthy child and lead a normal life. That is our commitment.”
Katiane Magarawa – Indigenous woman (Cacoal, Rondônia)
Katiane, from the Suruí people, is followed monthly by the DSEI health team, which brings prenatal care and rapid testing directly to her village. She sees testing as a form of protection for both herself and her baby.
“I trust the care. We do the tests to make sure everything is fine—it gives me security for myself and for my baby.”
Hanna Silva – Nurse, Specialized Care Service (Salvador, Bahia)
Every day, Hanna welcomes women who arrive with questions, fears, and often the emotional impact of an unexpected diagnosis. Her work goes beyond technical care—it is built on listening, trust, and health education. She acts as a bridge between primary health care and the specialized service, ensuring continuity of care from testing through specialized follow-up.
“Pregnant women arrive very afraid. We welcome them, explain everything, and walk alongside them. In the end, they realize they can have a safe pregnancy—and that they are not alone.”
Dr. Arlete Baldez – Head of Epidemiological Surveillance (AGEVISA, Rondônia)
Dr. Arlete coordinates epidemiological surveillance actions in Rondônia, closely monitoring every pregnant woman, every infant, and every service involved in preventing mother-to-child transmission of HIV. Her work connects primary health care, specialized services, maternity hospitals, and laboratory networks, ensuring that no woman or child is lost along the continuum of care. She explains that strengthening prenatalprenatal care, combined with active surveillance and coordinated action across services, was essential to protect mothers and babies.
“When everything works as a network—prenatal care, early diagnosis, timely treatment, and follow-up through the postpartum period—we can protect both the mother and the baby. Our goal is to reach 18 months and say: there was no mother-to-child transmission.”
Joelma Melchiades – Community Health Worker (Cacoal, Rondônia)
Joelma has worked for 20 years as a community health worker at the Cleide Gomes Basic Health Unit. She serves as a vital link between pregnant women and the health system, ensuring active case-finding, guidance, and continuity of care.
“Our role is very important. We actively seek out pregnant women because this care is essential—not only for them, but for the baby’s future.”
Jennifer – Pregnant woman receiving care (Cacoal, Rodônia)
Jennifer receives prenatal care at a Basic Health Unit in Cacoal, where rapid testing for HIV, syphilis, and hepatitis is part of routine care. For her, this first step is essential to ensure safety throughout pregnancy.
“I always tell other mothers: attend prenatal care. Testing gives peace of mind to continue the pregnancy safely—it’s health for the whole family.”