Mental, neurological and substance use conditions account for 14% of the burden of disease. Between 75-90% of people with these conditions do not receive the treatment they need even though effective treatment is available; this represents the existing mental health gap.
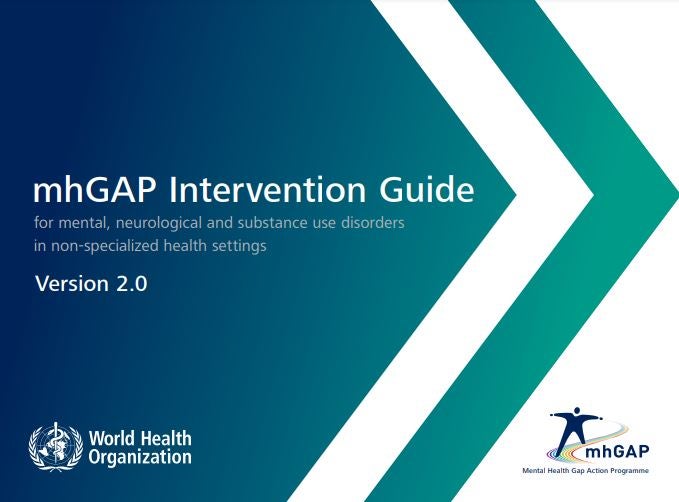
The Mental Health Gap Action Programme (mhGAP) aims to address the unmet needs of people with mental, neurological and substance use conditions in non-specialized health services.
Common mental health conditions can be managed from primary care. The integration of mental health is a key strategy that countries must include in their mental health model.
This strategy is committed to a new comprehensive and integrated, accessible and quality mental health model, from a health service network approach, facilitated by coordination and referral, monitoring and support from the specialized level.
- Between 75–90% of people with mental, neurological and substance use disorders do not receive the necessary treatment despite the existence of effective treatment, this represents the gap in mental health.
- The estimated treatment gap for schizophrenia in the Region of the Americas is 72%.
- Mental, neurological and substance use disorders represent more than one third of the total years lived with disability (YLD) and one fifth of the disability adjusted life years (DALYs) in the Region of the Americas.
- Alcohol consumption is also prevalent in the Region, with 8.2% of the population over 15 years of age having alcohol use disorders.
- Every year, 93,337 deaths by suicide are registered in the Region, which represents a rate of 9.0 per 100,000 inhabitants, with significant variations between countries and subregions of the Americas. The regional suicide rate has increased by 17% since the year 2000.
- Median public spending on mental health across the Region is barely 3% of the health budget, and more than 43% of this money goes to psychiatric hospitals, while community-based services are underfunded.
- There is only a median of 14.9 mental health workers for every 100,000 inhabitants in the Region, which reveals the need to increase the number of trained health professionals to improve the provision of services.
The primary care approach to mental health is based on a community approach that emphasizes promotion, prevention, social participation, health services organization and liaison with other services as well as the recovery of people in their environment. It proposes a transition from the seclusion of people with mental problems in
psychiatric hospitals to dignified and quality care in the community. This is referred to as the process of deinstitutionalization.
Recovery-oriented care emphasizes empowering people to manage their own lives. It involves supporting people to find hope, build self-esteem and resilience, establish healthy relationships, regain independence, and live a life that is meaningful to them.
Cross-cutting principles for the integration of mental health into primary care
Universal health coverage: promoting that all people have access to the full range of quality health services they need, when and where they need them, without financial hardship.
Human rights: to promote the rights and defend the dignity of people with mental health problems.
Evidence-based practices.
Life course and people-centered approach.
Multi-sectoral approach: in alliance between health, education, protection, justice, and private sectors, among others.
Empowerment of people with mental conditions and psychosocial disabilities through their inclusion in decision-making about care and services.
PAHO began its support to the countries of the region for the integration of mental health in primary care in 2010 with a training and pilot project in Panama. Since then, it has been accompanying countries so that they have non-specialized health professionals with the necessary skills to attend to mental health problems in primary care and specialized personnel with the skills to train and supervise non-specialized personnel.
Since 2019, PAHO's technical cooperation has focused on accompanying countries to develop operational plans for the implementation of the mhGAP strategy and a roadmap to facilitate it. The essential steps are:
PLANNING
- Creation of an mhGAP operational team with key actors.
- Situational analysis of the prevalence and burden of mental health problems, the capacity of services and available personnel, and the treatment gap.
- Development of an operational plan that includes all actions to be carried out, with responsible persons and allocated funding.
PREPARATION
- Adaptation of the different components of the mhGAP package to the local sociocultural context.
- Development of a training plan for health care providers that includes materials, people to be trained, logistics and modality.
- Clinical supervision plan that includes modality and tools.
- Creation of a monitoring system with indicators, tools, responsible persons, and frequency.
- Strengthening of referral and counter-referral systems between different health care levels and sectors.
- Ensuring access and continuous availability of psychopharmacological treatment and psychological
interventions. - Establishing mechanisms for the availability of time during mental health care consultations.
PROVISION
- Provision of mental health services in primary care facilities, in a coordinated and complementary manner with specialized mental health care levels.
- Integration of mental health promotion and prevention actions.
- Awareness-raising actions on mental health for health personnel, decision-makers and communities.